As the globe continues to navigate our irreparably changed, post-COVID world, we persist in the face of debilitating anxiety. Yet we wonder: Could it happen again?
While no one is yearning for the nostalgic, halcyon days of 2020-2022, the universe seems to be steering us back towards challenging times in public health. This is particularly evident with the recent emergence of a troubling situation in Shanghai. A new form of pneumonia–highly infectious in children–is making headlines, but it's not an isolated issue.
In fact, this surge in pediatric pneumonia cases is being directly attributed to a widespread outbreak of RSV (respiratory syncytial virus) in China. The virus is causing severe respiratory issues, contributing significantly to emergency situations in pediatric care across the country.
So, what does the savvy survivalist need to know to prepare for another potential pandemic? What role does drug resistance play? And how are children especially susceptible?
Dust off your Schitt’s Creek DVDs, stock up on toilet paper, and get ready to bake some more bread–here we go again?
Sometimes it do be that way. (Image courtesy of Rockstar Studios)
Table of Contents
-
01
China’s RSV Surge
-
02
Walking with pneumoniae
-
03
Pediatric vulnerabilities
-
04
They’re Evolving
-
05
Preventing a new pandemic
-
06
Final words
-
07
Frequently Asked Questions
China’s RSV Surge
Since mid-October, the World Health Organization has been keeping an eye on China. Worrying reports about a potential new, drug-resistant RSV disease caught the attention of multiple officials. This prompted the Chinese National Health commission to confirm these anxieties in a press conference held on November 13.
At this press briefing, Chinese authorities confirmed that there was an uptick in the incidence of respiratory diseases, specifically ones that were predominately afflicting children.
Initially, Chinese officials credited this RSV surge to relaxing COVID-19 precautions and restrictions during the arrival of flu season. They reported that well known pathogens such as influenza, pneumonia (mycoplasma pneumoniae) RSV, and severe acute respiratory syndrome (SARS-Cov-2) were making their typical seasonal rounds.
However, about a week later on November 22nd, the World Health Organization caught wind of multiple clusters of undiagnosed pneumonia in children’s hospitals in major Chinese cities.
Assumedly, the WHO felt a way about this, and submitted an official request to China to provide additional clinical information, as well as lab results from the afflicted patients–hoping to gain some insight into whether this surge of pneumonia cases was widespread, isolated, or simply misreported.
Shortly after requesting this information, Chinese health authorities delivered an underwhelming statement, which, in summary, stated: “There’s an uptick in sick children from multiple illnesses, but it’s cold season here so that’s normal; there’s no new viruses coming out of the woodwork, and our hospitals are not being overwhelmed.”
Notably, the WHO’s risk assessment for the region is currently fairly low. Let’s break down the quick facts:
🔶China is actively experiencing a surge in common, well-known diseases during cold season.
🔶These diseases have tested treatments.
🔶Hospitals are not overwhelmed, but they are packed.
🔶Chinese officials aren’t sounding any alarms, and neither is the WHO.
Something else of importance to mention is that the U.S. in 2022 saw a similar “outbreak” when COVID-19 restrictions were relaxed. During this time, COVID, RSV, and influenza all spiked in much the same way we’re seeing in China.
Phew–that’s great news! Have we avoided a new pandemic? If everything holds steady, we should be in for smooth sailing… right?
Potentially, yes. Except we need to discuss what these “common” diseases are, because while they may be making their usual rounds, they carry significant dangers.
Firstly, these diseases are being reported specifically among pediatric patients–a startling fact for any parent. Possibly more worrisome, however, is the emerging information about drug resistance regarding mycoplasma pneumoniae.
Emeritus Professor of Paediatric Pulmonology Ioannis Tsanakas claims m.pneumoniae has mutated to resist nearly 90% of available drugs on the market today.
We’ll explore the emerging threat of drug resistances later. But before that, let’s talk about m.pneumoniae specifically, and why it could have devastating effects if we don’t adhere to the lessons learned from COVID-19.

Mycoplasma pneumonia (Image courtesy of Steve Gschmeissner, via Science Photo Library)
Walking with pneumoniae
Mycoplasma pneumoniae are bacteria that cause illness through damaging of the respiratory system’s mucous linings. Often the throat, lungs, and windpipe are affected, resulting in sore throat, fatigue, fever, cough, and headache. This bacteria can cause different types of infections:
-Tracheobronchitis: This form of bronchitis caused by mycoplasma pneumoniae results from heavy inflammation of the trachea and bronchi (lung structures). Its effects are characterized by cough, fever, and purulent sputum (hacking up mucus).
Tracheobronchial infections are usually acquired from a hospital setting, especially one when ventilators are highly utilized, often in an intensive care unit.
Referred to as ventilator-associated tracheobronchitis, it is not to be confused with fungal and herpetic tracheobronchitis, which result from fungal and herpes simplex complications.
This means this infection is normally a secondary complication when treating a patient for chronic obstructive pulmonary disease, or other ventilator-necessary treatments calling for the use of a breathing tube.
If you’ve ever put your furry friends up in a kennel or animal-hotel, and they returned home with the dreaded “kennel cough,” your pet was likely afflicted by a variant of tracheobronchitis called canine infectious tracheobronchitis.
-Pneumonia: Pneumonia is an infection of a lung or both lungs in which the alveoli of the lung are filled with pus and other liquid. While pneumonia refers to any form of liquid in the lungs, such as drowning, it is more commonly understood to be caused by bacteria or viruses.
For today’s purposes, we’ll be referring to mycoplasma pneumonia. This illness is considered to be atypical, as the bacterium it stems from causes slightly different symptoms than normal pneumonia.
To be specific, m.pneumonia–also referred to as walking pneumonia–will present as less severe than typical pneumonia. The issue, as it were, is that with walking pneumonia, an infected person is much less likely to seek medical care as a result of lessened symptoms… initially.
The devil is in the details, as walking pneumonia will creep up on its victim, and can leave an individual in a rough place.
Severe complications of m.pneumonia can cause or worsen underlying issues like:
🔶 Serious pneumonia
🔶 Ear infections
🔶 Asthma
🔶 Encephalitis (brain swelling)
🔶 Anemia
🔶 Renal disease
🔶 Skin rashes
When put into this perspective, it’s easy to see why a child could be quickly overwhelmed by such a sneaky infection. Little kids, after all, are usually fairly sick–touching toys, drooling on everything, not understanding why a lego that has been inserted into their friend’s nose is no longer suitable consumption: the normal stuff.
But what exactly makes children so susceptible to becoming sick in the first place? While it may seem obvious–they’re gross–there is, of course, a bit more to it.

Children are more susceptible to illness than adults are. (Image courtesy of Coastal Kids, A Paediatric Medical Group)
Pediatric vulnerabilities
While many school teachers will tell you that children are essentially “bowling balls with feet” or “little adults,” the former isn’t exactly correct from a physiological standpoint.
Without stating the obvious too much–they’re smaller and younger. This means their immune systems are immature and haven’t had time to develop. While our immune systems have survived sickness, infection, and Chipotle, many children have not.
Indeed, children are constantly being exposed to new and exciting ways to get sick. Every day brings a new discovery via curiosity: “Can I put the cat’s tail in my mouth?” “What happens when I lick the dishwasher door?” and “If Peppa Pig doesn’t have to take a bath, why do I?”.
That’s why, as adults, it’s our job to gently guide our little bowling balls with feet in the right direction. But we can’t be with them 24/7, even though sometimes we wish we could (and sometimes we wish school days were longer).
At school or daycare, young kids are intensely susceptible to sickness. Children don’t always realize it’s advisable to cover their mouth when coughing, or to wipe their nose when they sneeze instead of rubbing it all over a table or doorknob. While this in and of itself isn’t a pediatric emergency, it could lead to one down the road.
This is especially relevant given that children’s upper airways aren’t fully developed, which puts them at risk for more frequent and viral/bacterial infections.
While children are bad at following directions, they’re also not entirely to blame for their constant illness. Children’s bodies also use energy quicker than adult’s do, which means they need to eat and drink water more frequently. Seeing as both of these activities require physical touch–you can see where this is going: it’s a numbers game.
Additionally, kids have much thinner skin and a higher resting respiratory rate. Smaller hearts and muscles means their little bodies have to work much, much harder to profuse oxygen.
Thinner skin, meanwhile, can be credited for children absorbing more chemical or biological matter, and a higher respiratory rate contributes directly to inhaling and exhaling potential viruses at an accelerated rate.
One other factor to consider is that kids simply aren’t very good at communicating. While the occasional toddler may mention that another child went home early or seemed unwell during the school day, many toddlers may think nothing of it.
When your typical day consists of pooping your pants, vomiting from eating too many goldfish, and trying to forcibly retrieve snacks from locked drawers, it’s hard to really narrow down which topic of discussion you’re going to unleash on your parents first.
All this to say, children may also only mention that they “feel tired.” As any new mother will tell you, kids are an enigma. Sometimes they’re just tired; sometimes they don't eat the PB&J you packed (just the crusts); and occasionally they’re just moody little bundles of joy.
Kids can’t always come right up and say: “Hey I’ve been feeling unwell for about two to three weeks; a classmate has been absent with pneumonia for a while; and I found this lightsaber under the bed.”
Alright, they might say that last part, but the rest might not make it to you.
Although children may be resistant to bringing their concerns to their parents, this resistance pales in comparison to certain microbes and their resistance to antibiotics.
Please, hold your applause, and wash your hands.
On that note, let’s clarify some of the surging illnesses present in China, and lightly touch on why antibiotic resistance may turn the tide in favor of bacterias.
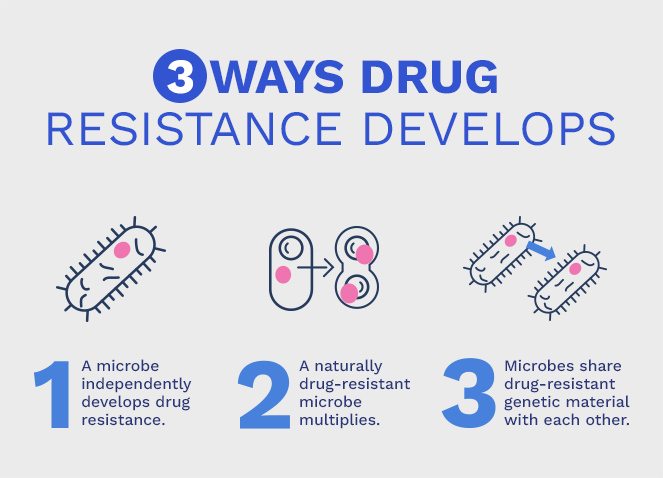
Drug resistance in three easy steps. (Image courtesy of Psomagen)
They’re Evolving
China’s RSV surge places many onlookers in a curious place. With so many illnesses being thrown around, it’s important to clarify some terminology:
🔶 Influenza: The common flu we all get each year, and get shots for.
🔶 RSV: Viral infections, normally referred to as the common cold.
🔶 Mycoplasma pneumoniae: Bacteria-caused illness.
🔶 SARS: Severe acute respiratory syndrome, associated with COVID.
As we know, all of the illnesses listed above are respiratory complications. Each one can also present with mild or severe symptoms. The common cold is most people’s immediate assumption at the first sign of feeling unwell.
Many of us will reach for a bottle of Dayquil and press on with our day. However, China’s RSV surge may prove to obfuscate important details of one’s health. With the RSV surge in full swing during China’s cold season, many children and adults may feel fairly comfortable with avoiding the doctor.
This is a primary breeding ground for walking pneumonia, as it presents very closely with RSV symptoms. When we all know there is “something going around,” and then we get sick, we’re obviously going to assume it’s that “something.”
The gamble now, though, is that it could be any one of four illnesses currently surging through China, as they all present very similarly. We’re just hoping it’s not walking pneumonia, and we hopefully don’t suffer from underlying symptoms that may lend themselves to exacerbation.
It’s not just the obvious complications from m.pneumoniae we need to worry about though, it’s the concerning information surrounding its growing drug resistance.
Significantly, a survey consisting of 158 hospital executives, conducted by the Sepsis Alliance, found that 90% of these organizations all agree: drug resistance is a threat to society.
Antimicrobial resistance, or AMR, is a global concern according to the WHO, who states that bacteria resistance is rising in seventy-six countries. While lack of sanitation, cleanliness, and access to clean food and drinking water will exacerbate and drive pathogens to mutate, it doesn’t mean first-world countries are safe.
In much the same way evolution of animals works, bacteria will respond to external stimuli and evolve. One such method is through selective pressure, or “survival of the fittest”: Bacteria with resistant genes live, and bacteria that may be defeated with antibiotics perishes.
As the bacteria multiplies and passes on these resistant genes, we find ourselves facing quite the conundrum. If we’re sick, we need antibiotics, right? While this is true, treating any and all illness with antibiotics only serves to strengthen their gene pool.
Way back in the 1940s, a study was done within the first decade of penicillin trials that uncovered a shocking 50% resistance among a bacteria called staphylococcus aureus. That’s how fast these resistances can form.
Luckily, up until now, modern medicine has managed to outpace bacterial evolution. The WHO worries that, at some point, however, a microbe may gain the upper hand.
M.pneumonia, notably, currently sports a 90% resistance against antibiotics in Asian countries. The U.S. and Europe have also reported growing resistance, but at around 10%.
So, with all that said, should we be worried? The answer is a resounding: “Maybe.”

Hope you saved a few! (Image courtesy of Oklahoma State University)
Preventing a new pandemic
While it shouldn’t be controversial to say “wear a mask when you’re sick,” we live in 2023. Whether or not you agree with laws mandating wear, it’s simply foolhardy to undercut the benefits of masks when it comes to preventing the outbreak of the next pandemic.
Normal masks like the N95, do a great job of filtering out large and small particles during exhaling and inhaling. This greatly reduces the chance of contracting an illness, as most airborne contagions are spread via vapor particles.
Of course, less refined masks like hand-crafted ones or medical masks are still important and should be considered as they will still filter out large particles, and prevent a fair amount of your own from spreading to others.
Then, we have our MIRA Safety masks. These are for your “no-fail” plans. When it absolutely must work the first time, and continue working every time, these are what you need for your family.
Remember: your children are your legacy, your flesh and blood, and the most important thing you are charged with protecting as a caregiver and parent.
They deserve the best–so give them the best.



Don’t be that guy. (Image courtesy of Care.org)
Final words
During the early days of the 2020 COVID-19 pandemic, many people found themselves beset by shock, awe, and in some cases, denial. While the scope of this article cannot possibly hope to address COVID-19 denial, we can stick to the facts.
The facts are:
COVID-19 was real. COVID-19 killed people who were young, old, and otherwise compromised. COVID-19 exposed many government’s lack of planning, response, preparation, and ability to operate efficiently when subjected to the overwhelming enormity of a global pandemic.
While we may have wanted it to go away, like a miracle, it didn’t. With that said, masks were effective in stymying the spread of COVID-19, and masks are still effective at reducing the spread of diseases.
We, as survivalists, cannot in good conscience see a potential epidemic or pandemic in its infancy and turn a blind eye–though it may be tempting to do so. Indeed, this writer once scoffed at the notion of needing to have a pandemic preparedness kit.
“If I’m ready to counter chemical weapons, I should be ready to counter a cold,” he thought.
He was wrong. He had a miserable time, and many people around him also had a miserable time. Luckily though, he didn’t have any small children around.
Kids change you. They alter the way you look at the world, the way you conduct yourself, and the amount of small bags of snacks you have to carry around.
They also serve to pluck our heartstrings–specifically the strings that awaken our inner guardian. A good guardian does whatever it takes to ensure their little ones live a happy and healthy life–even if their offspring insist on eating dirt.
Granted, MIRA Safety can’t stop your kids from eating dirt. But, we can offer top-of-the-life solutions to emerging problems facing our world today.
As of the time of this writing, there’s no indication we’re facing another global pandemic. However, someone probably said this same thing during the early stages of COVID-19 as well. Only time will tell what comes next–but we can be better prepared than last time.
Stay savvy, survivalists.

